Diseases of the Retina
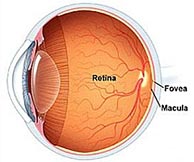
Retinal diseases specifically affect the retina — a layer of tissue at the back of the eye that is responsible for vision. These diseases can affect the retina, the macula (area of central vision), or the fovea at the center of the macula. Many retinal diseases share common symptoms and treatments, but each has unique characteristics.
AGE-RELATED MACULAR DEGENERATION
Retinal diseases specifically affect the retina — a layer of tissue at the back of the eye that is responsible for vision. These diseases can affect the retina, the macula (area of central vision), or the fovea at the center of the macula. Many retinal diseases share common symptoms and treatments, but each has unique characteristics.
Nonproliferative Diabetic Retinopathy

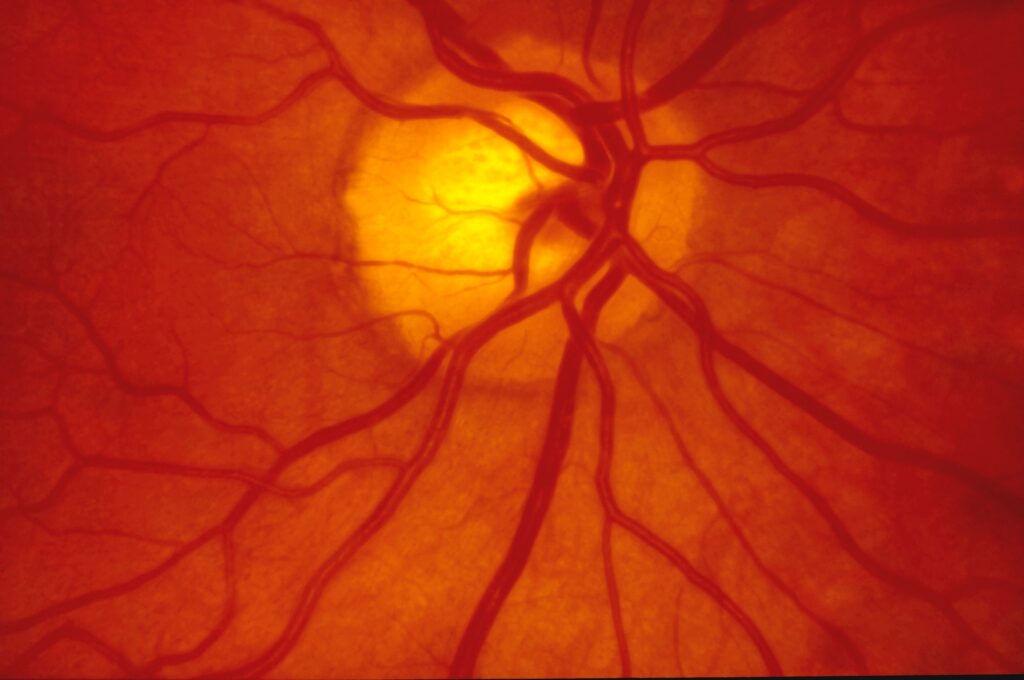
If you have diabetes mellitus, your body does not use and store glucose properly. Over time, diabetes can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Proliferative Diabetic Retinopathy

Proliferative diabetic retinopathy (PDR) is a complication of diabetes caused by changes in the blood vessels of the eye. If you have diabetes, your body does not use and store sugar properly. High blood sugar levels create changes in the veins, arteries, and capillaries that carry blood throughout the body. This includes the tiny blood vessels in the retina, the light-sensitive nerve layer that lines the back of the eye.
Detached and Torn Retina
A retinal detachment is a very serious problem that usually causes blindness unless treated. The appearance of flashing lights, floating objects, or a gray curtain moving across the field of vision are all indications of a retinal detachment. If any of these occur, see an ophthalmologist right away.
locations
Charlottesville
620 Berkmar Circle | Charlottesville, VA 22901
Phone: 434-220-3420
Mon-Fri: 8am-5pm
Fishersville
17 N. Medical Park Drive | Fishersville, VA 22939
Phone: 540-213-7484 | Fax: 540-213-7729
Mon-Fri: 8am-5pm
CONTACT US
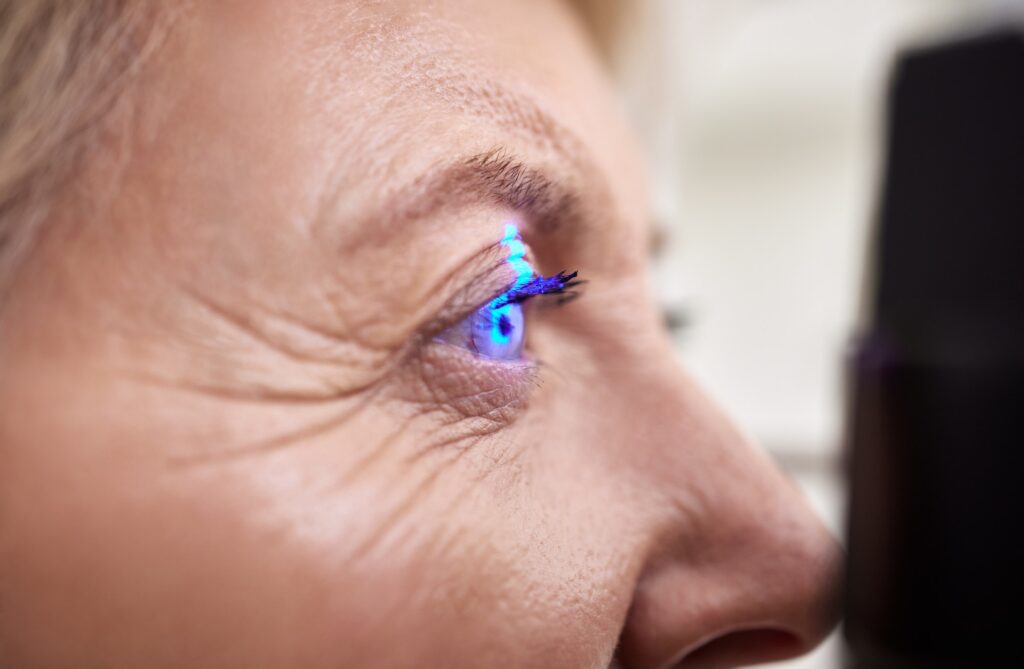
If you suffer from any of the signs or symptoms listed, call RetinaCare of Virginia today to schedule your consultation.
